Leventhal’s Self-Regulatory Model of Illness Behaviour
Understanding How Individuals Respond to Illness
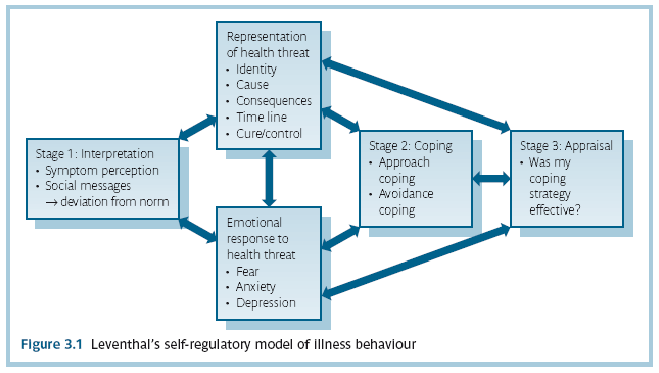
Illness is a fundamental human experience, yet individuals interpret and respond to health threats differently. Leventhal’s Self-Regulatory Model of Illness Behaviour (SRM), developed in 1984 by Leventhal, Nerenz, and Steele, provides a structured framework for understanding how individuals perceive, react to, and manage their illnesses. The core premise of the model is that people are motivated to regulate their health-related risks and take actions that align with their perceptions of a health threat. In essence, individuals develop cognitive representations of their illness, engage in coping strategies, and continuously appraise their progress in managing their condition.
The SRM is composed of three key stages:
Stage one (Representation – interpretation of threat)
The first stage involves how an individual perceives and understands a health threat. This is based on personal experiences, external information (such as medical advice), and cultural beliefs. Each person forms a unique cognitive representation of their illness, influencing how they approach coping and treatment.
Second stage (coping – appropriate action)
Once an illness is perceived, individuals take steps to manage their health condition. Coping strategies can be problem-focused (such as taking medication, following a treatment plan, or making lifestyle changes) or emotion-focused (such as seeking social support or using denial to manage distress). The chosen coping strategies depend on how the illness is perceived and the resources available to the individual.
Third stage (appraisal – monitoring progress)
In the final stage, individuals evaluate the effectiveness of their coping strategies. They may modify their coping mechanisms if their initial approach does not alleviate symptoms or improve their health. This self-regulation process continues until they feel a sense of control over their condition or reach a point of acceptance.

Five dimensions of illness representation
Leventhal’s model further breaks down illness perception into five dimensions that shape how individuals interpret their condition :
Dimension 1 (Identity – disease label and symptoms)
The identity dimension involves how individuals define their illness, including the name of the condition and its associated symptoms. For example, a person experiencing persistent coughing and breathlessness may label their condition as a “cold” or “asthma,” depending on their prior knowledge and experiences. The accuracy of this self-diagnosis influences whether they seek professional medical advice or attempt self-treatment.
Dimension 2 (Cause – perceived origins of the illness)
People often seek to understand what caused their illness. Causes may be attributed to biological factors (such as genetics or infection), behavioural factors (such as smoking or poor diet), or external factors (such as environmental pollution or stress). The perceived cause influences how individuals approach treatment: for example, someone who believes stress causes their migraines may focus on relaxation techniques rather than seeking medication.
Dimension 3 (Timeline – duration and course of illness)
The timeline dimension refers to how long an individual expects their illness to last. Acute diseases (such as the flu) are often perceived as short-term, whereas chronic conditions (such as diabetes) are seen as long-term or permanent. If someone believes their illness is temporary, they may be less likely to commit to long-term management strategies. Conversely, those who see their disease as chronic may adopt an ongoing coping strategy.
Dimension 4 (Consequences – impact on life)
The perceived consequences of an illness play a crucial role in shaping behaviour. If a person believes their condition will severely impact their daily life, work, or relationships, they may be more likely to seek treatment or lifestyle changes. Alternatively, if they perceive the illness as minor and inconsequential, they may neglect medical advice, leading to poorer health outcomes.
Dimension 5 (Cure/Control – perceived ability to manage the illness)
The final dimension involves believing whether the illness can be cured or controlled. Individuals who believe they control their condition through medication, lifestyle changes, or medical interventions are more likely to engage in proactive health behaviours. However, if they perceive their illness as uncontrollable or untreatable, they may experience feelings of helplessness, leading to avoidance or resignation.

The role of illness representations in Health behaviour
Illness representations influence a wide range of health behaviours, including:
Seeking medical help – Individuals who recognize their symptoms as severe and chronic are more likely to seek professional healthcare.
Treatment adherence – Beliefs about cure and control affect whether individuals follow prescribed treatments or use self-management strategies.
Lifestyle changes – Those who perceive their condition as serious and modifiable may be more inclined to adopt healthier behaviours such as exercise and dietary changes.
Psychological well-being – Misinterpretations of illness (e.g., seeing a chronic condition as untreatable) can lead to anxiety, depression, or avoidance behaviours.

Applications of the Self-Regulatory Model
SRM has been widely applied in various health psychology and medical research areas. Some key applications include:
Chronic disease management
For individuals living with chronic illnesses such as diabetes, asthma, or heart disease, the SRM helps explain how they adapt to long-term health challenges. Understanding how patients perceive their condition allows healthcare professionals to tailor interventions that improve adherence to treatment and self-care practices.
Health communication and patient education
Healthcare providers can use the model to improve patient communication. By addressing misconceptions about illness causes, timelines, and consequences, medical professionals can help individuals better understand their health conditions, leading to better decision-making and treatment adherence.
Mental health interventions
Individuals with chronic illnesses often experience psychological distress. The SRM provides insight into how illness perceptions contribute to emotional responses such as anxiety or depression. Cognitive-behavioural therapy (CBT) can be used to reframe maladaptive illness beliefs and promote more effective coping strategies.
Public health campaigns
The model has been used in public health initiatives to encourage health-promoting behaviours. For example, campaigns promoting cancer screening often address illness representations by emphasizing early detection’s role in improving outcomes and control.
Conclusion
Leventhal’s Self-Regulatory Model of Illness Behaviour offers a comprehensive framework for understanding how individuals interpret, respond to, and manage health threats. By recognizing the importance of illness representations and the self-regulation process, healthcare professionals can develop more effective interventions that align with patients' perceptions and needs. Whether applied in clinical practice, health education, or public health initiatives, the SRM remains a valuable tool for promoting positive health behaviours and improving patient outcomes.
Ultimately, how we perceive illness significantly impacts our approach to health management. By understanding and addressing these perceptions, we can encourage individuals to take control of their health and improve their overall well-being.